Breast Cancer: Understanding Treatment with Radiotherapy
Welcome to our dedicated page on breast cancer. Breast cancer management is multidisciplinary, involving surgery, chemotherapy, hormonal therapy, targeted therapy and radiotherapy. In particular, we’ll delve into the role of radiotherapy in combating breast cancer.
Overview of Breast Cancer:
Breast cancer is a type of cancer that forms in the cells of the breast, often starting in the ducts or lobules. It is one of the most common cancers affecting women worldwide, but it can also occur in men. Early detection and advancements in treatment have significantly improved outcomes for individuals diagnosed with breast cancer.
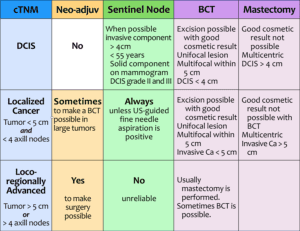
image source: radiology assistant
Types of breast cancer
Luminal A: estrogen/progesterone positive, low ki-67 –> endocrine therapy, or consider multi-gene risk testing. consider chemotherapy if high risk
Luminal B: as above but HER-2 enriched, high proliferation index –> chemo, then endocrine
Triple-negative: low threshold for chemotherapy, consider neoadjuvant approach
Her-2 enriched: targeted therapy, consider neoadjuvant approach
The Role of Radiotherapy:
One crucial aspect of breast cancer treatment is radiotherapy. This form of treatment is commonly employed after surgical procedures like lumpectomy or mastectomy. Radiotherapy can be to the breast or chest wall, or to the regional lymph nodes. Find out more about regional lymph node irradiation.
The primary goals of radiotherapy in breast cancer treatment include:
Elimination of Residual Cancer Cells:
Following surgery, there may be microscopic cancer cells left behind. Radiotherapy helps eliminate these remaining cells, reducing the risk of recurrence.
Risk Reduction:
By strategically using radiation, healthcare professionals aim to decrease the likelihood of cancer returning to the treated area, thereby enhancing overall survival rates.
Tumor Shrinkage and Symptom Alleviation:
In cases where breast cancer has advanced, radiotherapy can be employed to shrink tumors or alleviate symptoms, contributing to an improved quality of life for the patient.
Post-Surgery Radiotherapy:
After a lumpectomy or mastectomy, radiotherapy is often recommended to ensure a more comprehensive approach to treatment. This adjuvant therapy plays a pivotal role in preventing the cancer from coming back and is an integral part of many breast cancer treatment plans.
Post-neoadjuvant chemotherapy:
In some instances, especially when the tumour is more advanced or is of a special subtype ( e.g. triple negative or HER-2 enriched), chemotherapy is given before surgery to shrink the tumour. In some patients who achieve complete response after chemotherapy, radiotherapy may be omitted. But in patients with residual disease, or have certain risk factors despite complete response, radiotherapy is still administered. Find out about radiotherapy after neoadjuvant chemotherapy.
Whole breast
Partial breast
Boost
Regional nodes
Process of radiotherapy:
Treatment Planning:
The radiation oncologist works with medical physicists and dosimetrists to develop a customized treatment plan. This plan considers the size and location of the tumor, as well as the surrounding healthy tissues.
Advanced technologies such as three-dimensional conformal radiation therapy (3D-CRT), intensity-modulated radiation therapy (IMRT) or VMAT may be used to precisely target the cancer cells while minimizing exposure to normal tissues.
Treatment Sessions:
Breast radiotherapy is typically delivered on an outpatient basis, meaning patients do not need to stay in the hospital.
Treatment sessions are usually scheduled daily, Monday through Friday, for several weeks (1 to 4 weeks depending on stage and type of radiotherapy). The total number of sessions varies depending on the specific treatment plan and the type of breast cancer.
Radiation Delivery:
Patients lie on a treatment table, and the radiation therapy machine is carefully aligned to target the breast area. The patient should remain as still as possible during the treatment.
The actual radiation delivery is a quick process, usually lasting only a few minutes. Patients are not radioactive after treatment, and they can go about their normal activities.
Side Effects:
Common side effects of breast radiotherapy may include fatigue, skin changes (such as redness or darkening), and mild discomfort. These side effects are generally temporary and can be managed with proper care.
The radiation oncology team monitors the patient’s progress and addresses any side effects that may arise during the course of treatment.
If your cancer is on the left, you may be asked to hold your breath in order to minimize heart radiotherapy dose.
Collaborative Approach to Treatment:
Breast cancer treatment is highly personalized, and decisions about radiotherapy are made collaboratively between the patient and their healthcare team. Factors such as the stage of cancer, the type of surgery performed, and individual health considerations play a crucial role in determining the most effective treatment strategy. Consider joining a local breast cancer support group to learn more. Find out more about Breast Cancer Support Groups.