Cancer and Radiotherapy Education
Cancer Types
Find out more about the treatment of different types of cancer using radiotherapy.
Radiotherapy types
Read more about various kinds of radiotherapy (proton, VMAT, SRS etc).
Radiotherapy Techniques
Proton therapy, VMAT, 3D, Electrons, IMRT, SBRT, SRS, Brachytherapy
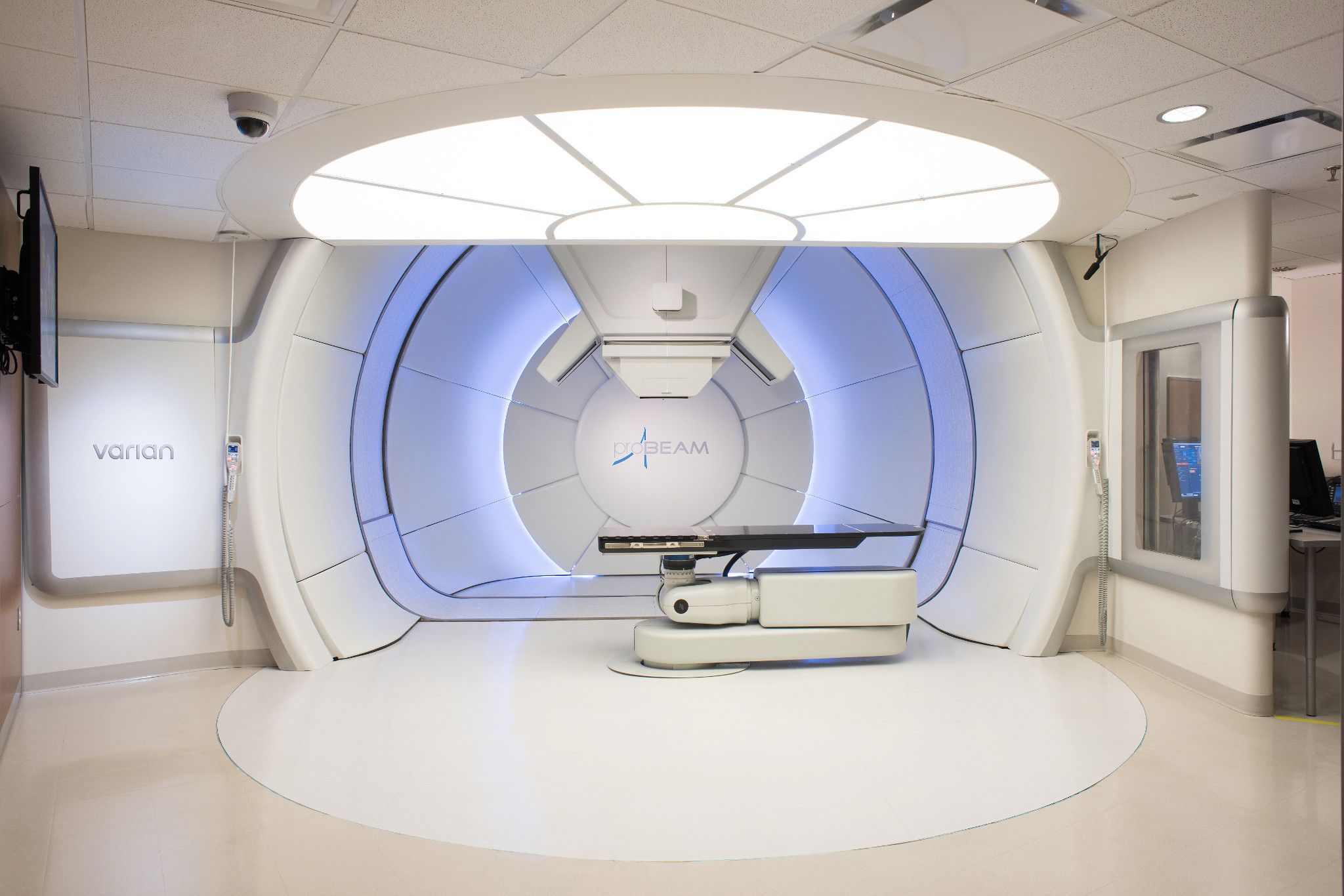
Proton therapy
Proton beam therapy is a form of radiotherapy that uses protons, positively charged particles, to precisely target and treat cancer cells, with minimal exit dose in normal organs, distal to the tumour.
Download Proton-Beam-Therapy-A-patient-Guide

- Minimise dose distal to tumours
- Allows for high doses to tumours
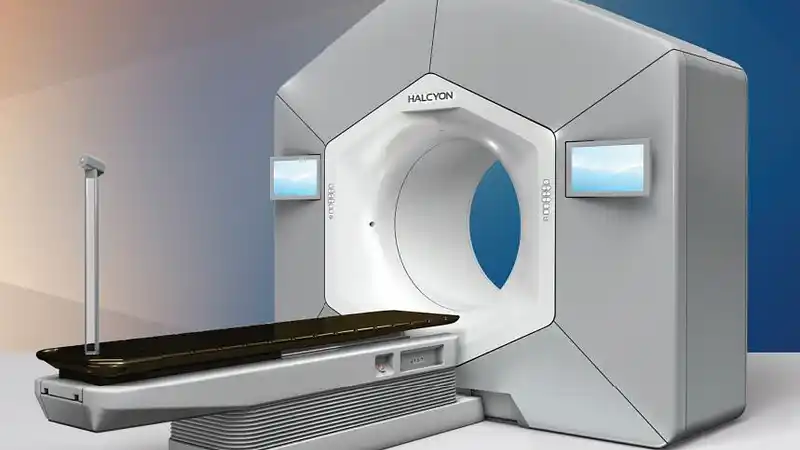
Volumetric Modulated Arc Therapy
VMAT radiotherapy uses x-rays that are shaped to form a conformal treatment target. It is known for its shorter treatment times, increased treatment accuracy, and improved sparing of critical structures, contributing to more effective and patient-friendly radiation therapy.
- Modulated
- Comfortable
Stereotactic Ablative Radiotherapy or Radiosurgery
Stereotactic Radiosurgery (SRS), or ablative body radiotherapy ( SABR, SBRT etc) is a non-invasive and highly precise radiotherapy technique used to treat small tumors or lesions in the brain or other parts of the body.
- Concentrated
- 1-5 fractions
- Highly accurate
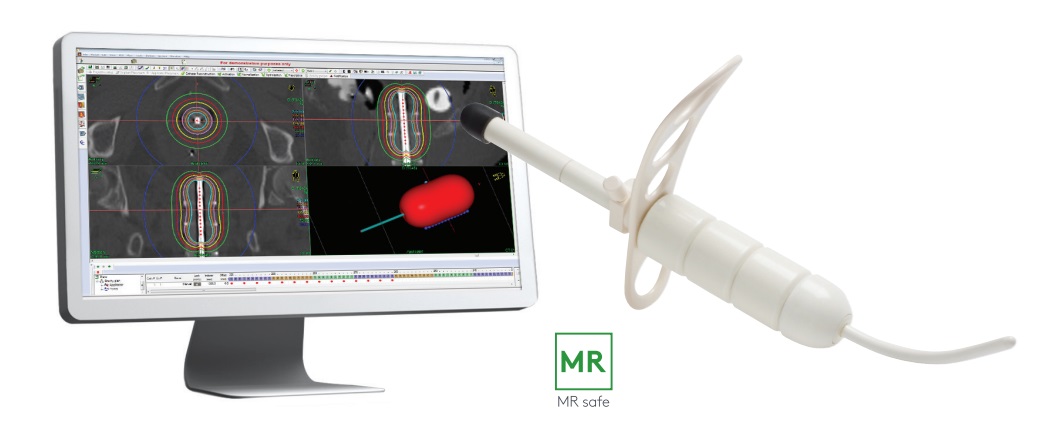
Brachytherapy
Brachytherapy is a type of internal radiation therapy used to treat cancer by placing a radioactive source directly inside or next to the tumor, usually into a body cavity. It is more commonly used in gynecological cancers. This allows a high dose of radiation to be delivered to the cancer while minimizing exposure to surrounding healthy tissue. Brachytherapy is effective, targeted, and often associated with shorter treatment times and fewer side effects compared to external radiation.
How is proton different different?
Proton therapy is a type of radiation therapy that uses protons rather than traditional photons. Protons have unique physical properties that allow for more precise targeting of tumors, with the potential to reduce damage to surrounding healthy tissues.
Read about which cancers can be treated with proton beam therapy.
When is proton therapy used?
Unlike traditional X-ray radiation, protons deposit their energy more precisely, minimizing damage to surrounding healthy tissues. This precision is particularly beneficial in treating tumors located near critical structures or in pediatric patients, where sparing healthy tissues is crucial. Proton therapy is often employed in various cancers, including brain tumors, prostate cancer, head and neck cancers, liver cancers, and certain pediatric malignancies, with the goal of maximizing treatment effectiveness while minimizing side effects.
Understanding Cancer: Knowledge is Power
Radiotherapy technology is very advanced these days, leveraging complex computer software and complex linear accelerator to deliver treatment ranging from proton therapy, to high dose ablative radiosurgery, to radionuclides sources placed directly near tumours (brachytherapy).
What is radiotherapy?
Radiotherapy, also known as radiation therapy, uses high doses of radiation to kill or damage cancer cells, preventing them from growing and dividing.
What are the potential side effects of radiotherapy?
Radiotherapy, like many cancer treatments, can cause side effects. The specific side effects can vary depending on the type and location of the cancer being treated, the dose of radiation, the duration of treatment, and individual patient factors. It’s important to note that not everyone will experience the same side effects, and some individuals may have minimal side effects.
How can patients manage the side effects?
For short term toxicities, medications and lotions can be given to patients. For long term toxicities, prevention is key. Your radiation oncologist will explain these to you and review you along the way.
What is the process of radiotherapy?
Referral and Consultation:
Simulation involves the use of imaging techniques (such as CT scans) to identify the tumor and surrounding normal tissues.
Immobilization devices may be used to help the patient maintain a consistent position during treatment.
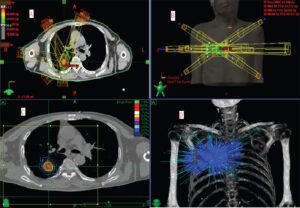
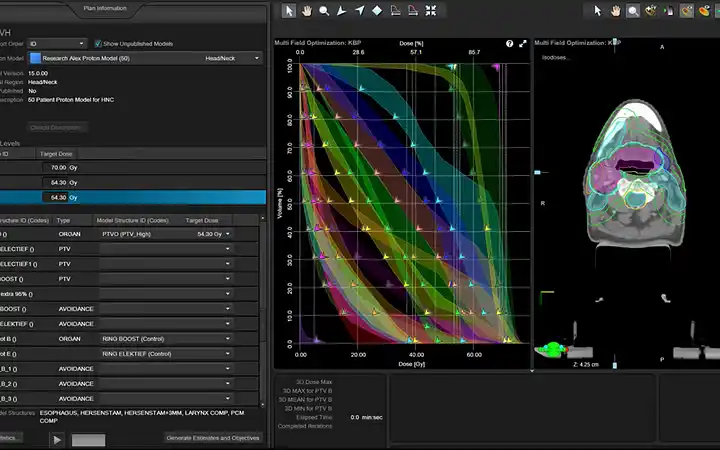
Treatment Planning:
The radiation oncology team, which includes medical physicists and dosimetrists, uses the simulation data to develop a treatment plan.
Treatment planning involves determining the appropriate radiation dose, the angles from which the radiation beams will be delivered, and the duration of treatment.
Quality Assurance:
Before actual treatment begins, the treatment plan undergoes a rigorous quality assurance process to ensure accuracy and effectiveness.
Treatment Sessions:
The patient undergoes a series of treatment sessions, typically scheduled daily from Monday to Friday.
Each session is relatively short, lasting only a few minutes, although the overall treatment duration varies depending on the type and stage of cancer.
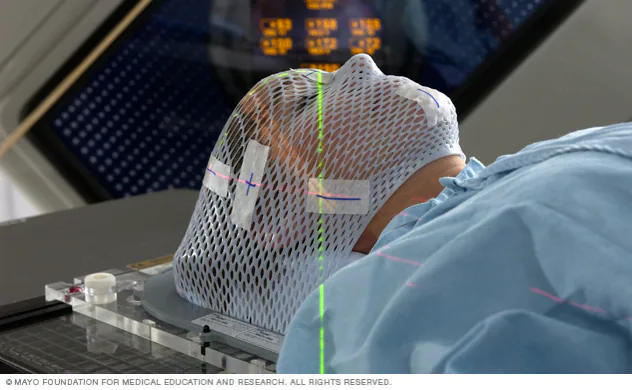
Positioning and Immobilization:
Before each treatment session, the patient is carefully positioned on the treatment table using the immobilization devices established during simulation.
Image-guided techniques may be employed to verify the precise positioning of the patient.
Delivery of Radiation:
The patient lies on the treatment table, and the linear accelerator or other radiation delivery system is used to deliver targeted radiation beams to the predetermined treatment area.
The radiation therapist operates the equipment from a control room, monitoring the process through imaging and computer systems.
Monitoring and Adjustments:
Throughout the course of treatment, the radiation oncology team monitors the patient’s response to therapy.
If necessary, adjustments to the treatment plan may be made to account for changes in the tumor size or location.
Side Effect Management:
Throughout treatment, the healthcare team works closely with the patient to manage and alleviate any side effects.
Supportive care measures may include medications, skincare recommendations, and nutritional guidance.
Follow-Up Care:
After completing the prescribed course of radiotherapy, the patient continues to receive follow-up care to monitor the treatment’s effectiveness and address any potential side effects.
How do patients monitor their cancer progress after radiotherapy?
Via clinical examination and imaging modalities like CT, MRI, PET-CT and sometimes blood cancer markers.

Breast Cancer
Radiotherapy is used after breast conserving surgery, or after a mastectomy in selected patients. Modern radiotherapy is very safe and well tolerated. Breath-holding radiotherapy can further reduce heart doses.

Gastrointestinal and Liver Cancer
For rectal cancer, neoadjuvant radiotherapy, with or without chemotherapy, can reduce the risk of recurrence.
For liver cancers, SBRT can ablate small metastases and primary disease. Protons is a useful tool for unresectable hepatocellular carcinomas.

Lung Cancer
In advanced lung cancers, radiotherapy can be used concurrently with chemotherapy to control the tumours. In small cancers, stereotactic body radiotherapy can be used to ablate the tumours with more than 90% efficacy.

Paediatric Cancer
Radiotherapy is an integral component of paediatric oncology. However, late-onset toxicity can be a major concern. Proton therapy helps to mitigate the risk of late-onset toxicity.

Prostate Cancer
Prostate cancer can be treated very safely with Stereotactic Body Radiotherapy, or proton therapy in selected cases.
Patients with a few distant metastases can also receive ablative radiotherapy to these areas.

Nasopharyngeal Carcinoma
Modern treatment for NPC is safe and efficacious. Proton therapy can further reduce side effects.
For locally recurrent NPC, repeat radiotherapy is an option in some patients.

Brain Tumours
Benign brain tumours like acoustic neuroma and craniopharyngiomas can be controlled safely with moderate doses of radiotherapy. Brain tumours like gliomas can be managed with surgery, chemotherapy and radiotherapy. Small brain metastases can be eradicated with stereotactic radiosurgery.

Sarcomas
Radiotherapy is delivered to the surgical bed with image-guidance treatment with pre-operative MRI guidance. For selected tumours near critical organs, proton therapy can provide safe and high probability of control, e.g. chordoma. For unresectable tumours, high doses of proton therapy can be used to cure.
Process of radiotherapy
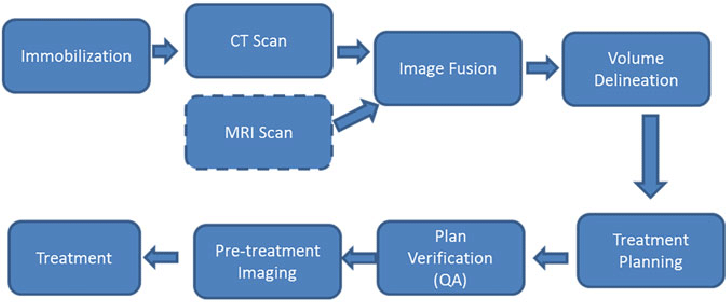
- After consultation, the patient will undergo a series of procedures.
- Radiotherapy preparation is a painless process, involving immobilisation and image-acquisition (simulation).
- The radiation oncologist then draws out the tumour to be treated and normal organs to be avoided.
- A physicist or radiation therapy then uses advanced computer algorithms to calculate the doses and most optimal angles for treatment.
- The radiation therapist will set the patient up and take on-couch images to ensure accuracy.
- While on the couch, the patient lie still for about 30 minutes or less. The process is painless.

Talk to your radiation oncologist about your treatment plans to discuss probabilities of short and long term toxicities, with mitigation strategies.

Modern radiotherapy is safe.

Updates
Get the latest news on radiotherapy and cancer discoveries.