Cervical Cancer Patient Education
Cervical cancer has been declining due to vaccinations and screening; however, it is still a public health problem.
Abnormal cervical pap smear or a positive high-risk HPV test should lead to colposcopy and biopsy or excisional procedures such as loop electrosurgical excision and conisation.
The World Health Organization (WHO) recognizes three categories of epithelial tumours of the cervix:
- squamous,
- glandular (adenocarcinoma) and other
- epithelial tumours including adenosquamous carcinoma, neuroendocrine tumours and undifferentiated carcinoma.
Squamous cell carcinomas account for 70%–80% of cervical cancers and adenocarcinomas for 20%–25%.
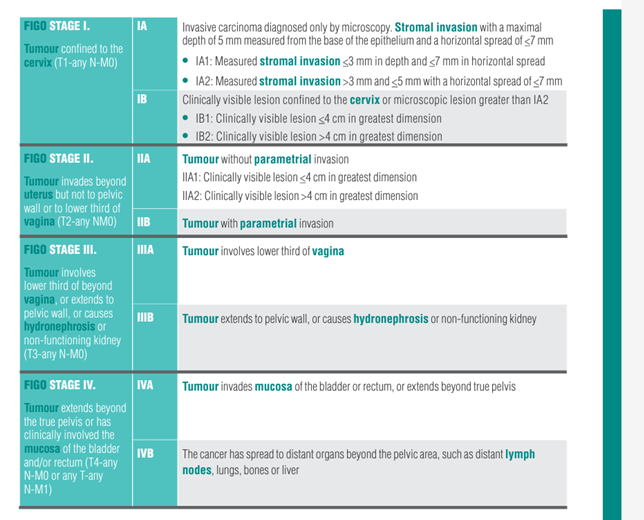
Staging
For in-situ
cancers, the management is conization ( removal of part of the cervix).
For early-staged invasive cancer, surgery is done for FIGO stage I to II cervical cancer
- Standard surgical management would be radical hysterectomy with bilateral lymph node dissection with or without sentinel node
- Open surgery has been shown in a few studies to have better cancer control than minimally invasive radical hysterectomy
For more advanced disease, radiotherapy with concurrent chemotherapy is recommended.
For patients with metastatic disease, chemotherapy with or without immunotherapy and targeted therapy is given, with local radiotherapy given to control symptoms.

Radiotherapy should be completed within 50 days if possible, and consists of external beam radiotherapy and brachytherapy.
Chemotherapy and EBRT are omitted on days with brachytherapy. Brachytherapy is done towards the end of EBRT. EBRT is given over 5 weeks, with or without a boost to the lymph nodes if they are involved.

Brachytherapy consists of 3 to 5 sessions
- The targets would the the original tumour and cervix.
- Patient would be sedated, and have a catheter inserted into the bladder, while brachytherapy channels are inserted into the cervix.
Side effects of radiotherapy include
Acute:
Nausea, skin irritation, bladder irritation, diarrhea
Long term:
Vaginal dryness and stenosis, which can be prevented with vaginal care
Cystitis (irritation and/or bleeding) from the bladder
Proctitis (irritation and/or bleeding) from the rectum
Lymphedema (if the pelvic lymph nodes are removed)
Early menopause (as the ovaries will stop functioning after radiotherapy)
Follow up
- Physical follow-up with pelvic-rectal examination is necessary
- CT with or without PET should be carried out about every 3-6 months, then 6-12 months after 3 years. After 5 years, patients will return to annual population-based examinations.
Survivorship
- The diagnosis of cervical cancer can be overwhelming. Consider reaching out to support groups.
