Credits Johnson et al, Can J Surg
2023
The treatment of rectal cancer typically involves a multidisciplinary approach, combining surgery, chemotherapy, and radiation therapy.
For early-staged cancers, surgical options are local excision, low anterior resection or abdominal-perineal resection. Patients with risk factors may opt for additional chemotherapy or radiotherapy after surgery.
For higher stages, a neoadjuvant approach with chemotherapy and/or radiotherapy is recommended sometimes. For surgery, a total mesorectal excision with either low anterior resection or abdominoperineal resection is usually performed. Factors such as risk of distant metastases, local symptoms, patients’ medical status and local tumour/node stage will determine the approach of chemotherapy, radiotherapy and surgery sequencing.
Total neoadjuvant treatment (in which the chemo and radiotherapy are given totally before surgery) has been investigated in various clinical trials and research studies, and some evidence suggests potential benefits, including an increased rate of pathological complete response (no evidence of cancer remaining at the time of surgery) and improved disease-free survival.
The specific treatment plan depends on various factors, including the stage of the cancer, the patient’s overall health, and individual preferences. Here is an overview of the common treatment modalities for rectal cancer:
- Surgery:
- Local Excision: For very early-stage rectal cancer, a local excision may be sufficient. This involves removing the tumor and a small amount of surrounding tissue.
- Total Mesorectal Excision (TME): For more advanced cases, a TME is often performed. This surgery removes the entire rectum and nearby lymph nodes to ensure the complete removal of cancerous tissue.
- Chemotherapy:
- Chemotherapy may be recommended before surgery (neoadjuvant) to shrink tumors and make them more manageable for surgical removal.
- Postoperative (adjuvant) chemotherapy may be recommended to reduce the risk of cancer recurrence.
- The drugs used in chemotherapy for rectal cancer may include fluorouracil (5-FU), capecitabine, oxaliplatin, irinotecan, and leucovorin. Combinations of these drugs are often used to enhance effectiveness.
- Chemotherapy can be given orally (pills) or intravenously (injected into a vein). The specific regimen and dosage depend on factors such as the stage of cancer, overall health of the patient, and whether it’s being used in combination with other treatments.
- Radiation Therapy:
- Radiation therapy may be used before surgery (neoadjuvant) to shrink tumors and improve the chance of successful surgical removal.
- For patients who have local symptoms (pain, discomfort, bleeding, blockage etc), a short course of radiotherapy (1 week), followed by immediate surgery is an approach. Chemotherapy after surgery maybe necessary in higher risk patients.
- For patients who are not locally symptomatic and have a higher risk disease, long course radiotherapy (5 weeks or more) together with chemotherapy in the pre-operative setting, can help to reduce recurrence risks.
- Targeted Therapy:
- Some rectal cancers may express specific molecular markers that can be targeted with medications. Targeted therapies, such as cetuximab or bevacizumab, may be used in combination with chemotherapy.
- Immunotherapy:
- Immunotherapy is a rapidly evolving field, and some clinical trials are exploring its use in colorectal cancer. Immunotherapy drugs, such as pembrolizumab or nivolumab, aim to stimulate the immune system to recognize and attack cancer cells.
- Follow-up and Surveillance:
- Regular follow-up appointments are crucial to monitor the patient’s recovery and detect any signs of cancer recurrence early.
- Supportive Care:
- Treatment plans may also include supportive care to manage symptoms, side effects, and improve the patient’s overall quality of life. This may involve pain management, nutritional support, and counseling.
It’s important for patients to discuss their specific case and treatment options with their healthcare team, as individual circumstances can vary. The choice of treatment is often personalized based on factors such as the stage of cancer, the patient’s overall health, and their preferences.
Here are some key points about radiotherapy for rectal cancer:
- Types of Radiotherapy:
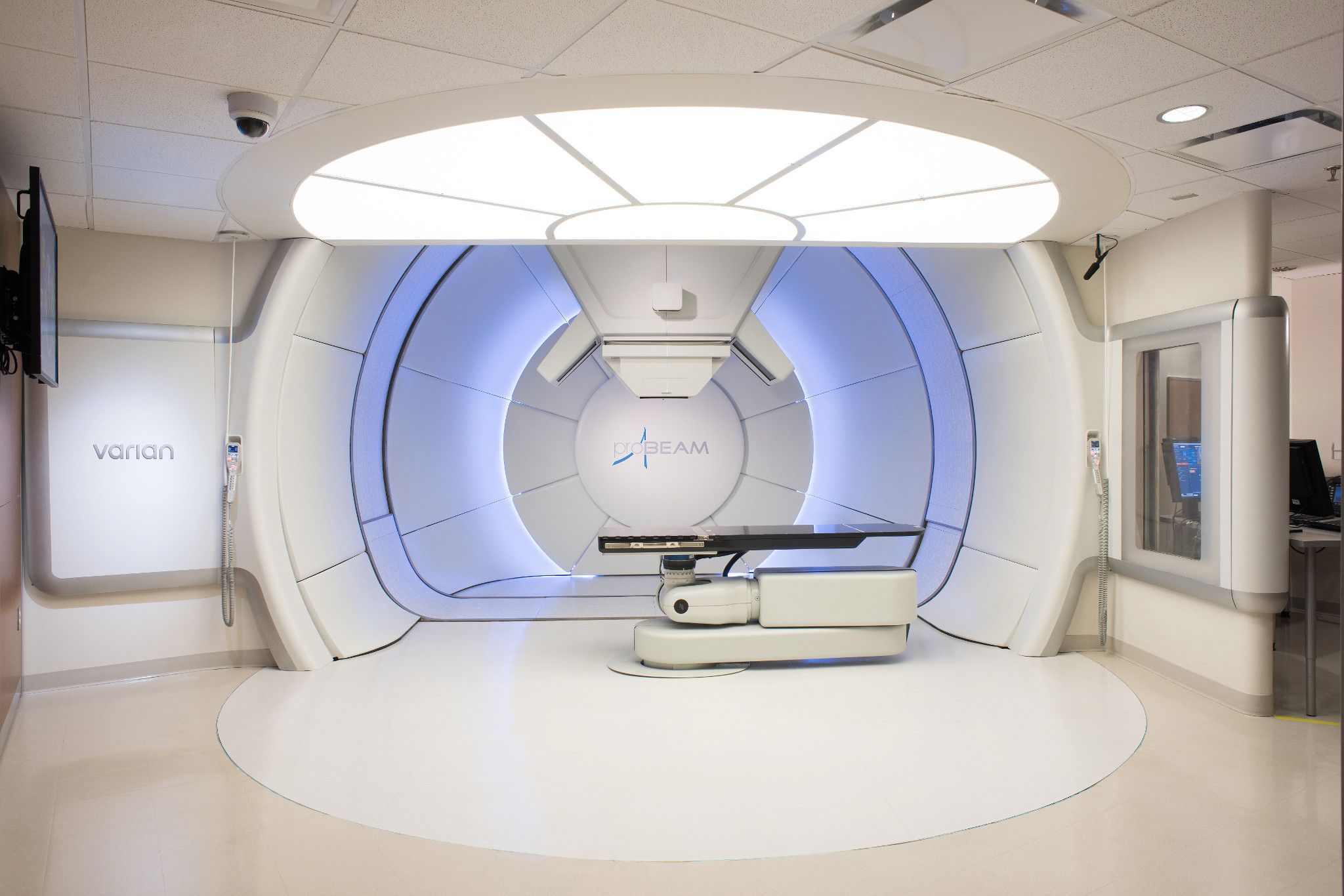
- External Beam Radiotherapy (EBRT): This is the most common type of radiotherapy for rectal cancer. It involves directing radiation from outside the body toward the cancerous tumor. The patient typically lies on a treatment table, and a machine delivers the radiation precisely to the targeted area.
- Internal Radiotherapy (Brachytherapy): This involves placing a radioactive source directly inside or very close to the tumor. This is not common and only given in very dedicated centers, especially when a boost radiotherapy dose is necessary to achieve organ sparing ( non-surgical approach).
- Treatment Planning:
- Before starting radiotherapy, a detailed treatment plan is developed. This includes imaging studies, such as CT scans, to precisely locate the tumor and determine the optimal angles for radiation delivery.
- Sessions and Duration:
- Radiotherapy is usually administered in multiple sessions, referred to as fractions. The total number of sessions and the overall duration of treatment depend on factors such as treatment regimen necessary ( short course 5# or long course with chemotherapy).
- Treatments are typically given daily over 1 to 5 or more weeks, allowing healthy cells to recover between sessions.
- Side Effects:
- Radiotherapy may cause side effects, and these can vary from person to person.
- Acute side effects for rectal cancer radiotherapy include fatigue, urinary frequency, and skin changes in the treated area.
- Long term side effects include scarring and bleeding.
- Most acute side effects are temporary and can be managed with supportive care.
- Combination with Other Treatments:
- Radiotherapy is often used in combination with surgery, chemotherapy, or both. The choice of treatment depends on factors such as the stage and type of lung cancer, as well as the overall health of the patient.
- Palliative Radiotherapy:
- In cases where the cancer is advanced and cannot be cured, radiotherapy may be used to relieve symptoms and improve the quality of life. This is known as palliative radiotherapy.
It’s important for individuals considering or undergoing radiotherapy for lung cancer to discuss the potential benefits and risks with their healthcare team, as well as to address any concerns or questions they may have about the treatment process
References
OPRA trial https://ascopubs.org/doi/abs/10.1200/JCO.23.01208 : clinical trial to investigate organ-preservation in rectal cancers for patients who respond well to neoadjuvant chemoradiotherapy and are willing to undergo close surveillance.
PROSPECT trial https://pubmed.ncbi.nlm.nih.gov/37272534/ : clinical trial for early and early-intermediate disease, comparing escalated/intensified chemotherapy alone versus chemoradiotherapy.
PRODIGE trial https://ascopubs.org/doi/10.1200/JCO.2023.41.17_suppl.LBA3504 : clinical trial for high risk patients, comparing neoadjuvant long course chemoradiotherapy with and without additional chemotherapy.
RAPIDO trial https://www.thelancet.com/article/S1470-2045(20)30555-6/fulltext: clinical trial for high risk patients, comparing short course radiotherapy, CAPOX/FOLFOX chemotherapy then surgery versus long course radiotherapy with oral chemo, surgery with or without post-operative CAPOX/FOLFOX.