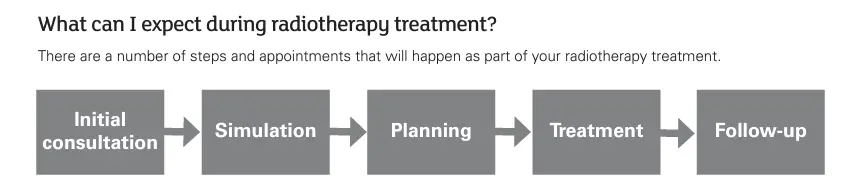
What is radiotherapy?
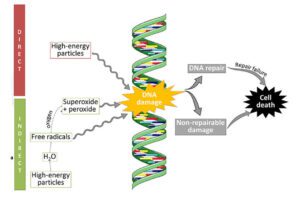
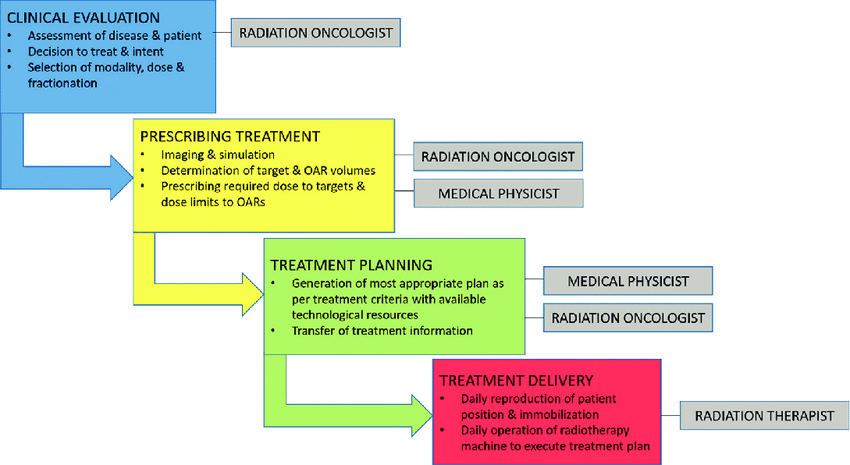
Radiotherapy involves the use of ionizing radiation to target and destroy cancer cells or shrink tumors.
Modern radiotherapy aims to maximize the effectiveness of treatment while minimizing damage to surrounding healthy tissues. Radiotherapy can be given externally, internally or with radionuclides.
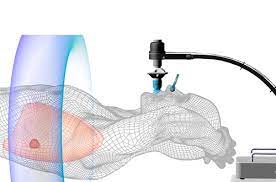
For head and neck, or brain treatments, a shell is customised to ensure treatment precision.


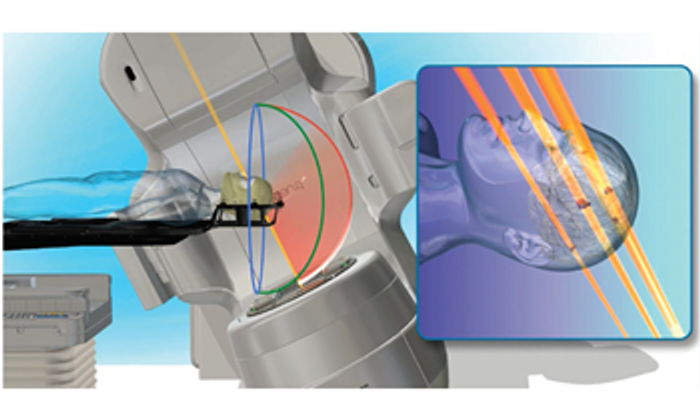
Proton beam Therapy & Intensity Modulated Proton Therapy (IMPT)
Proton Beam Therapy (PBT): uses high-energy sub-atomic particles called protons to precisely target tumours in the body while reducing radiation damage to surrounding normal organs and tissue. It is often used in the treatment of complex cancers such as in the head and neck, brain, liver, and in childhood cancers. It should be used in selected cases only as the technology is a lot more expensive than traditional x-ray technologies. Most cancers can already be safely treated with x-ray technologies like VMAT and IMRT.
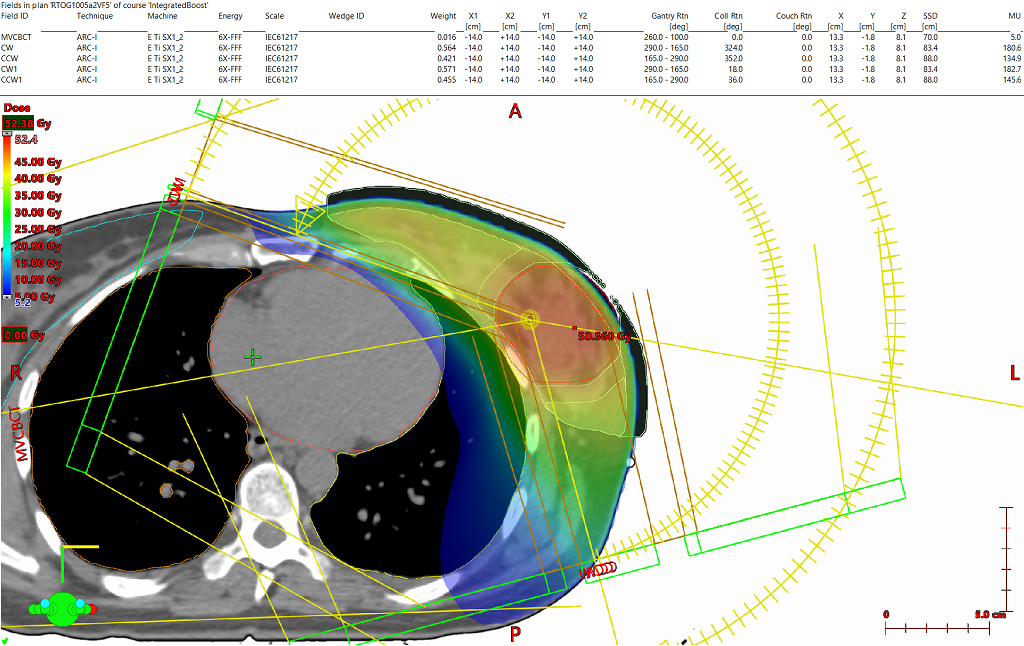
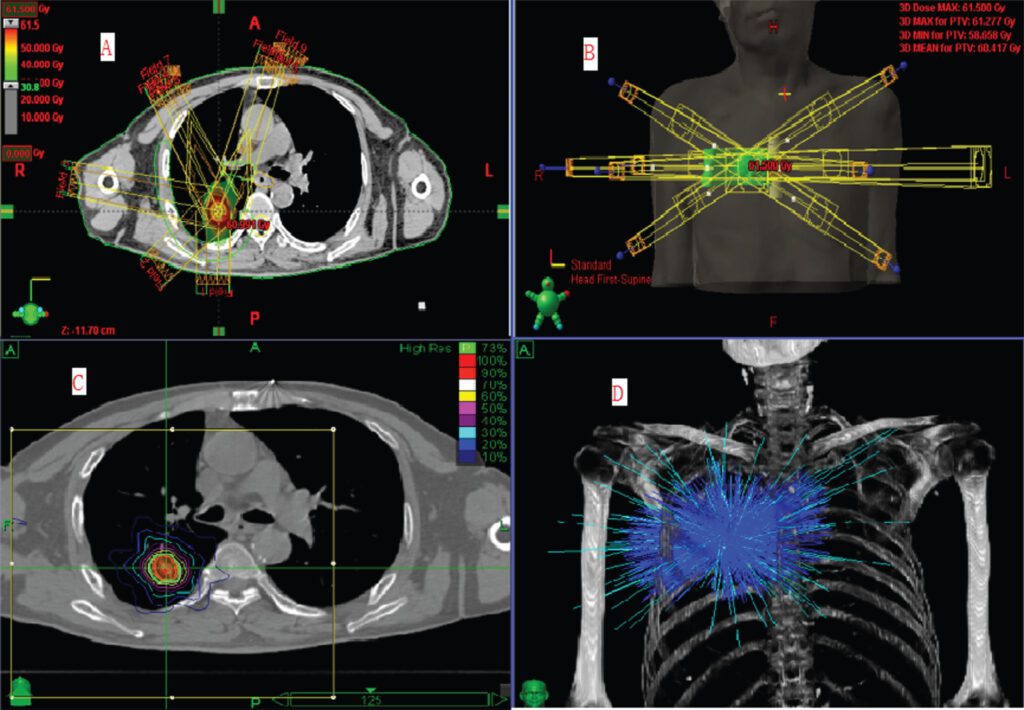
Newer technologies use strong magnets and complex computer algorithms to create a modulated plan for shaping of radiotherapy doses. These technologies and software, together with your radiation oncologists’ expertise, will customise a treatment plan that is an optimal combination of beam angles and intensities, creating a treatment that delivers the highest probability of tumour control balancing with normal organs toxicities.
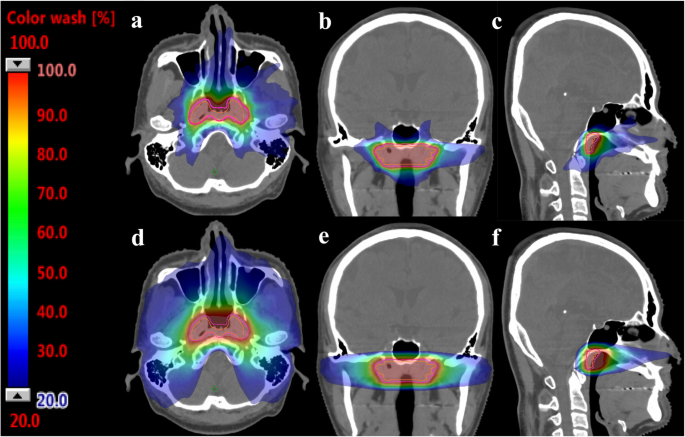

Intensity Modulated Radiotherapy (IMRT) & Volumetric Modulated Arc Therapy (VMAT)
Intensity Modulated Radiotherapy (IMRT): allows for the modulation of X-ray radiation beams in order to optimise target coverage and sparing of normal organs. This is achieved through the use of advanced computer algorithms and multiple radiation beams.
Volumetric Modulated Arc Therapy (VMAT): is similar to IMRT but instead of multiple fields, the treatment is delivered continuously in arcs, resulting in faster treatment times compared to IMRT.
Stereotactic Radiosurgery for brain Lesions
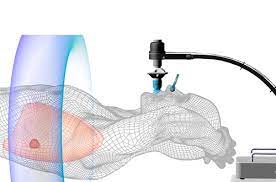
Stereotactic radiosurgery (SRS): is a non-invasive radiation therapy technique that delivers a concentrated dose of radiation to a precisely defined target in the brain, sparing normal tissues and killing cancer cells. SRS delivers a very high biological effective dose in a single or few sessions, which can result in better tumor control and reduced risk of recurrence.
Stereotactic Radiosurgery (SRS) delivers a single, high dose of radiation with sub-millimeter accuracy to a well-defined target, typically within the brain or spine. This is achieved using techniques like multiple non-coplanar beams, arcs, or sophisticated beam-shaping devices.
Unlike conventional radiotherapy, SRS is usually administered in a single session or a few fractions (up to 5).
Real-time imaging during treatment ensures that the radiation is precisely delivered to the target. SRS requires extremely rigid immobilization to maintain patient position during treatment.
Stereotactic Body Radiotherapy
Stereotactic Body Radiotherapy (SBRT): also known as stereotactic ablative radiotherapy (SABR), is an advanced radiation therapy technique that uses highly precise and concentrated radiation doses to kill cancer cells in various parts of the body such as the bone, lungs, kidney, and liver.

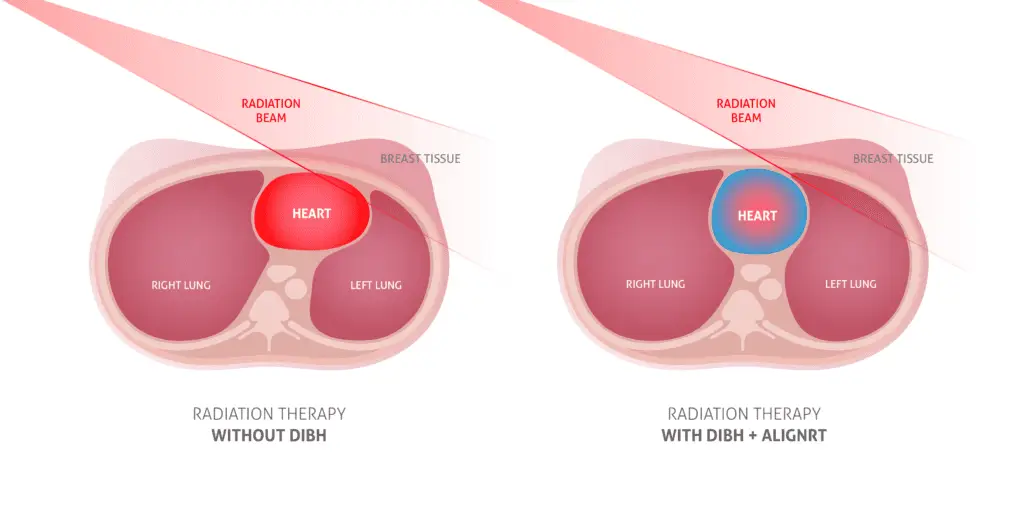
Breath-hold / Gating
Breath-hold and gating are techniques used in radiotherapy to manage the effects of patient motion, particularly respiratory motion, during treatment. These techniques help ensure that the radiation is accurately delivered to the target area while minimizing exposure to surrounding healthy tissues.
- Breath-Hold Technique:
- Purpose: The breath-hold technique involves having the patient hold their breath during specific phases of the respiratory cycle.
- Implementation: The patient is instructed to take a deep breath and hold it while the radiation is delivered.
- Advantages: By immobilizing the tumor during a breath-hold, clinicians can reduce the motion-related uncertainties
- Gating Technique:
- Purpose: Gating involves synchronizing the delivery of radiation with a specific phase of the respiratory cycle.
- Implementation: External markers or internal imaging (such as fluoroscopy or 4D CT scans) are used to monitor the patient’s breathing. Radiation is delivered only when the tumor is within a predefined position or range, known as the gating window.
- Advantages: Gating helps to account for variations in tumor position due to breathing, reducing the risk of irradiating healthy tissues.

Electrons
Electron radiotherapy is a type of external beam radiation therapy that utilizes high-energy electrons to treat cancerous and certain non-cancerous conditions. Electrons have a short range and is suitable for superficial tumours like skin tumours and cutaneous lymphomas. The process would require applicators and wax boluses to further shape and control the dose. Bolus materials are placed on the skin surface to ensure that the prescribed dose is delivered to the tumor.
3-Dimensional Radiotherapy

3D Conformal Radiotherapy: utilizes CT imaging to create a three-dimensional map of the tumor and normal organs in order to create a customized radiation treatment plan. Used commonly these days in straightforward breast radiotherapy, and in palliative indications for large tumours. The advent of 3D-CRT has paved the way for further developments in radiation therapy, such as intensity-modulated radiotherapy (IMRT) and volumetric-modulated arc therapy (VMAT)