- SAM RO
- 0 Comments

Cancer of the uterus/womb (endometrium) happens commonly in women after menopause. Its incidence is on the rise. The incidence of endometrial cancer varies geographically, with higher rates observed in developed countries. Risk factors include estrogen exposure, lifestyle and family risk etc.
Surger y is curative, and adjuvant treatment in the form of chemotherapy, external beam radiotherapy or brachytherapy is sometimes recommended.
Let’s learn about the staging of endometrial cancer.
Staging is an important aspect of diagnosing and determining the extent of cancer. Endometrial cancer staging is based on the International Federation of Gynecology and Obstetrics (FIGO) system.
Stage I: Cancer is confined to the uterus.
– Stage IA: The cancer is limited to the endometrium (lining of the uterus).
– Stage IB: The cancer has spread to less than half of the myometrium (muscle layer of the uterus).
Stage II: Cancer has spread to the cervix but remains within the uterus.
– Stage IIA: The cancer has spread to the cervical stroma (supporting tissue) but not beyond.
– Stage IIB: The cancer has invaded the connective tissue of the cervix.
Stage III: Cancer has spread beyond the uterus but remains within the pelvic region.
– Stage IIIA: The cancer has spread to the serosa (outer layer) of the uterus and/or ovaries and fallopian tubes.
– Stage IIIB: The cancer has invaded the vagina or parametrial tissues (tissues around the uterus).
– Stage IIIC: The cancer has spread to regional lymph nodes.
Stage IV: Cancer has spread to distant organs.
– Stage IVA: The cancer has spread to the bladder or rectum.
– Stage IVB: The cancer has spread to distant sites, such as the liver, lungs, bones, or distant lymph nodes.
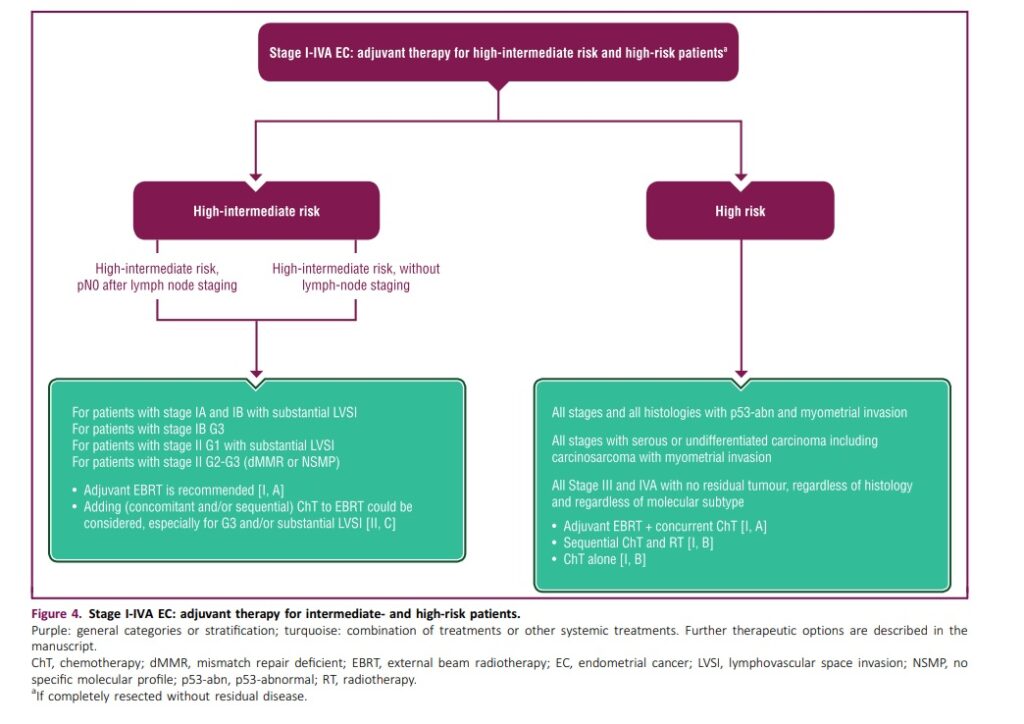
Risk groups are based on stage, lymphatic invasion, cancer mutation profiles and cancer types and grades.
- early
- Intermediate ( favorable and unfavorable)
- high

Low-risk group: Patients in the low-risk group have a favorable prognosis with a lower likelihood of disease recurrence. This group typically includes patients with the following characteristics:
– Grade 1 endometrioid adenocarcinoma: This is a well-differentiated form of endometrial cancer.
– Stage I disease: Cancer is confined to the uterus.
– No or minimal myometrial invasion: The cancer has not spread deeply into the muscle layer of the uterus.
– No lymphovascular invasion: There is no evidence of cancer cells in lymphatic or blood vessels.
– No or few risk factors: Absence of factors such as age over 60, obesity, family history of certain cancers, or history of hormone replacement therapy.
Adjuvant therapy may not be needed after surgery.

2. High-risk group: Patients in the high-risk group have a higher chance of disease recurrence and may require additional treatments. This group includes patients with one or more of the following characteristics:
– Grade 2 or 3 endometrioid adenocarcinoma: These are moderately to poorly differentiated forms of endometrial cancer.
– Stage II or higher: Cancer has spread beyond the uterus.
– Deep myometrial invasion: The cancer has invaded deeply into the muscle layer of the uterus.
– Lymphovascular invasion: Presence of cancer cells in lymphatic or blood vessels.
– High-risk factors: Factors such as older age, obesity, family history of certain cancers, or history of hormone replacement therapy.
Treatment for high-risk endometrial cancer often involves a combination of surgery, radiation therapy, and chemotherapy to reduce the risk of recurrence and improve overall outcomes.
Radiotherapy for endometrial cancer can be external ( using xrays from a linear accelerator ) or from internal ( brachytherapy, where radioactive sources are piped into a small cylinder to fit into the vaginal).
1. Treatment Planning:
– Prior to the procedure, the radiation oncologist will perform imaging tests, such as computed tomography (CT) or magnetic resonance imaging (MRI), to visualize the vaginal cuff and surrounding structures.
– The imaging helps determine the appropriate radiation dose and treatment length for the individual patient.
2. Applicator Placement:
– During the brachytherapy treatment, a specialized device called a vaginal cylinder or tandem and ovoids is used to deliver the radiation.
– The patient lies on a treatment table, similar to a pelvic exam, with her legs in stirrups.
– The vaginal cylinder or tandem, a hollow tube, is placed into the vagina and positioned so that the tip is at the level of the vaginal cuff.
3. Radiation Delivery:
– Once the applicator is in place, the treatment machine delivers the radiation to the vaginal cuff.
– The radiation oncologist and medical team typically leave the treatment room during the radiation delivery but can monitor the patient through audio and visual communication.
– The radiation source, which may be radioactive seeds or a high-dose-rate (HDR) brachytherapy machine, is inserted into the applicator and delivers the prescribed dose of radiation.
– The treatment time varies depending on the specific treatment plan, but it is usually a matter of minutes.
– The radiation source is then removed, and the applicator is taken out of the vagina.
4. Treatment Schedule:
– Endometrial vault brachytherapy is usually delivered over several sessions, known as fractions, with each session spaced apart, typically a few days to a week.
– The number of fractions and the total treatment duration depend on the specific case and treatment plan determined by the radiation oncologist.

For external beam radiotherapy
Treatment Planning:
- Prior to initiating external beam radiotherapy, a thorough treatment planning process is conducted. This involves imaging studies, such as CT scans, to precisely map the location and size of the tumor.
- Delivery of Radiation:
- The patient lies on a treatment table, and the radiation machine is adjusted to deliver the beams precisely to the targeted area. The process is usually painless, and each treatment session typically lasts a few minutes.
- The course of treatment may extend over several weeks, with daily sessions scheduled Monday through Friday.