Stereotactic body radiotherapy ( SBRT) is an effective option for patients with small non-small-cell lung tumours ( NSCLC) who are not suitable for surgery. It is also done to eradicate small relapses near the initial tumour after a lobectomy ( surgery for primary lung cancer). Even in patients with distant metastases, but experiencing good cancer control while on targeted or immunotherapy, SBRT can be given to areas of disease that are starting to progress to eradicate these clones so that patients can remain on current medications.

Traditionally, it is not administered with immunotherapy. On the other hand, immunotherapy is given in stage III NSCLC after chemoradiotherapy (Spigel et al JCO). A recently published trial reported early outcomes after studying the addition of immunotherapy after SBRT for early-staged lung cancers, or for local relapses after initial surgery.
In this trial, 156 patients with untreated stage 1A to stage IIB ( tumour smaller than 7 cm and node negative) lung cancer or cancer recurrence after surgery or chemoradiotherapy smaller than 7 cm were studied. They received SBRT with or without nivolumab (immunotherapy). After about 3 years, patients who had immunotherapy with SBRT had better tumour-free outcomes (77% versus 53%). No patients developed serious side effects from SBRT. In the patients who had immunotherapy, 15% of patients developed significant effects due to immunotherapy. None had side effects that resulted in death, or required hospitalisation.
The investigators in this study concluded that in patients who have early-staged initial lung cancer, or early recurrences suitable for curative treatment with SBRT, combining immunotherapy is safe and effective. However, more research is required to confirm this finding.
The process of radiotherapy:
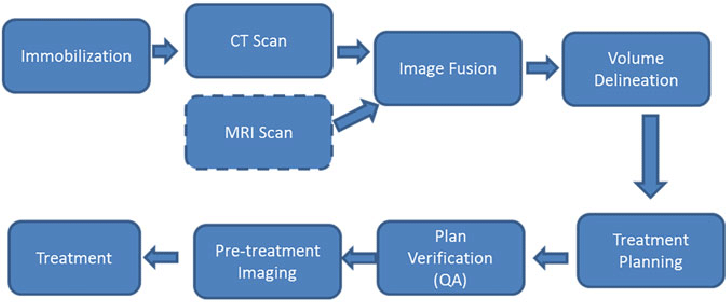
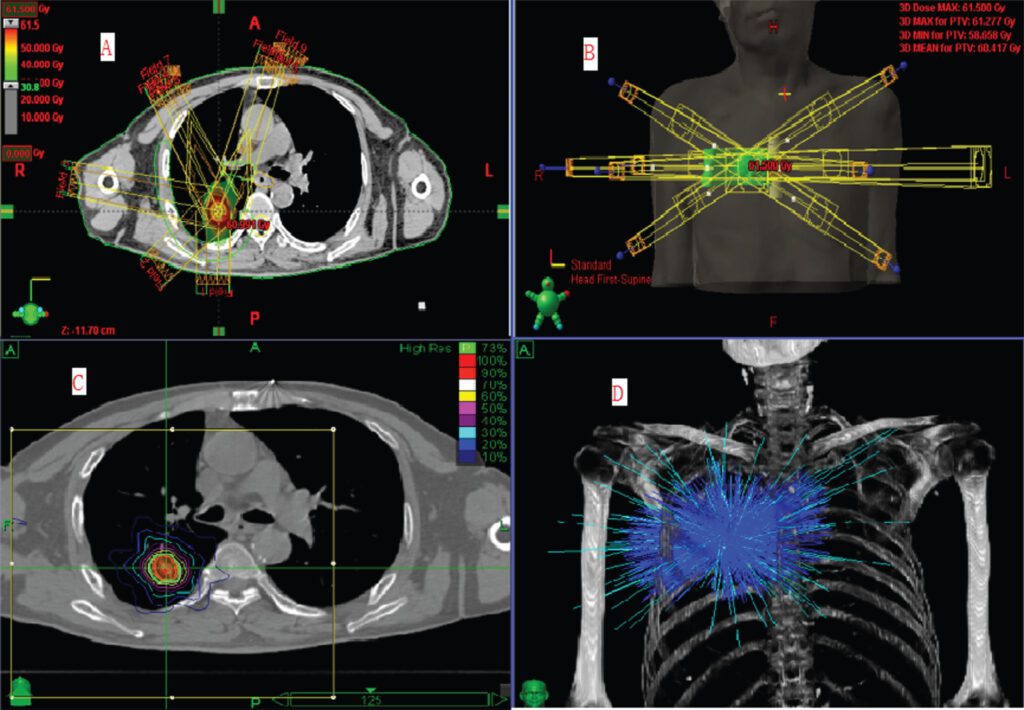
Before starting radiotherapy, a detailed treatment plan is developed. This includes imaging studies, such as CT scans, to precisely locate the tumor and determine the optimal angles for radiation delivery.
- During simulation, you may be asked to breathe slowly and regularly ( 4D CT scan) whereby your breathing cycle is imaged so that the tumour movement is tracked and delineated out for target planning.
- Sessions and Duration:
- Radiotherapy is usually administered in multiple sessions, referred to as fractions. The total number of sessions and the overall duration of treatment depend on factors such as the type and stage of lung cancer.
- Treatments are typically given daily over several weeks, allowing healthy cells to recover between sessions.
- For stereotactic body radiotherapy, treatments range from 1 to 5 sessions.
Dose fractionation for SBRT is dependent on site of tumour
- For small tumours far from critical organs and the chest wall ( ribs, muscles etc) : 3# x 18 Gy
- For tumours near the chest wall : 5# x 12 Gy
- For tumours near the central organs : 8# x 7.5 Gy
- Side Effects:
- Radiotherapy may cause side effects, and these can vary from person to person.
- Acute side effects for lung cancer radiotherapy include fatigue, difficulty swallowing, skin changes in the treated area and nausea.
- Subacute side effects include pneumonitis (inflammation of the lungs) which can be asymptomatic or cause shortness of breath. Usually this is temporary, but sometimes may require oxygen supplementation or steroids. For tumours near the main bronchus, a rare but life-threatening complication may happen if there is severe bleeding.
- Long term side effects include lung scarring, cardiac issues such as heart failure or ischemic heart disease.
- Most acute side effects are temporary and can be managed with supportive care.

