Surgery in oral cancers? Lower doses of radiotherapy for HPV cancers?
Oropharyngeal carcinomas can be caused by environmental factors (smoking, alcohol etc.) or viral-driven. Human papillomavirus (HPV) infection, a common transmitted disease, has been associated with the development of many cancers, including oropharyngeal squamous cell carcinoma (OPSCC) of the head and neck.
While traditional, environmentally related oral cancer rates have declined, there has been a dramatic rise in oral cancer related to high-risk types of HPV. Patients with HPV associated oral cancers that has not metastasized to distant organs typically have highly curable cancers and a better prognosis than those with non-HPV associated OPSCC.
Symptoms of oral cancer due to HPV are often different from traditional squamous cell carcinoma. HPV cancers tend to have lymph node involvement with neck swelling, and the primary tumours are often located more deeply in the throat, and less often in the oral cavity.
Prior to treatment with either surgery or radiotherapy, a few procedures should be undertaken. Patients should receive a complete dental evaluation, and nutritional assessment. Medications should be given to alleviate symptoms of the tumour and treatment. Although prognosis for HPV-related cancers is better, de-intensification of therapy (lower doses of radiotherapy), compared to conventional SCC, is still a subject of clinical trials.
For T1-2N0 tumours:
As HPV-cancers tend to present with node disease, most patients present with more advanced stage. But for selected patients with small primary tumours and node-negative disease, either surgery or radiotherapy is appropriate. A trans-oral approach, that is, a minimally-invasive one, should be carried out where appropriate. A thorough evaluation by an experienced, high-volume surgeon is needed to assess these possibilities, as surgical outcomes are superior with such surgeons. A clinical trial, ECOG-ECIN 3311 suggested excellent survival outcomes in patients with no nodal involvement (or one node without extranodal extension) treated with trans-oral robotic surgery (TORS) alone. However, in this trial, only a minority of patients received surgery alone. This is due to a high probability of patients requiring adjuvant chemoradiotherapy when neck node removal revealed metastases although initially thought to be negative.
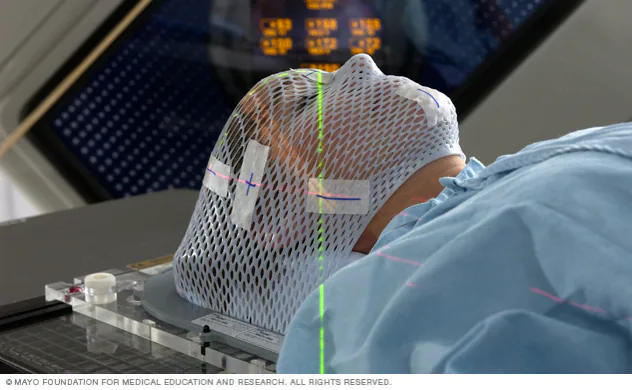
Another appropriate option is radiotherapy (RT) alone. RT is delivered to both the primary tumor and to cervical lymph nodes. RT is the preferred option for patients who are ineligible for surgery or who wish to avoid the potential complications of surgery, or in situations where expertise in trans-oral resection is not available.
For T1-2 and a single small involved node:
For non-smoking patients with one small single involved node ≤3 cm without adverse features on clinical evaluation and high-quality imaging (eg, no radiographic evidence of extranodal extension), single-agent RT is appropriate. Elective neck irradiation (to target lymph nodes) is often undertaken. Unilateral neck irradiation can be done if the tumour is small and not central. Patients with risk factors ( smokers, midline nodal involvement etc) should be offered chemoradiotherapy.
For patients with more locally advanced disease:
This includes a larger primary tumour, or multiple nodal involvement. Chemoradiotherapy alone, or trimodality (surgery, chemo and radiotherapy) are options, although the former offers organ-preservation. This is a controversial topic, especially in HPV-cancers, due to the sensitivity of these cancer cells to chemoradiotherapy and excellent outcomes with chemoradiotherapy.
Future steps:
Treatment de-escalation is being studied in larger studies to lower long-term toxicities from radiotherapy as these tumours have a good prognosis. Currently, the treatment intensity does not differ for HPV or traditional cancers, but this is the subject of multiple on-going trials. Proton therapy has the potential to lower side effects compared to X-ray therapy although long-term data is lacking. A recent study from New York with almost three hundred HPV-related oral cancer patients showed that between X-ray and Proton Beam therapy, tumour control was similar but during radiotherapy, patients had fewer side effects with proton, and a few months after treatment when early issues have resolved, dry mouth and severe eating problems were less with proton beam therapy. 95% of patients had no local recurrence after either X-ray or Proton Beam therapy.
References:
Uptodate.com
European Society Medical Oncology ( Pan-Asian adapted guidelines 2021)